Why this name?
If you are currently living with diabetes or supporting someone with the condition, you will be aware of the many numbers:
- Blood glucose levels
- HbA1c (average glucose levels over the past 3 months)
- Time in range
- Carbohydrate counting (how many carbs are in a food/meal)
- Insulin units
- Correction doses
In a professional capacity I was of course aware of blood glucose levels and HbA1c but I learnt about the others pretty quickly.
New technology that has been developed to support and manage Type 1 Diabetes such as continuous glucose monitors (CGM) and insulin pumps are life changing but they also mean that you are constantly surrounded by numbers, alarms, screens and target ranges. It can be overwhelming.
Whilst numbers are both important and essential, over the past 5 months we have started to learn that they are not everything. Numbers do not tell the whole story…
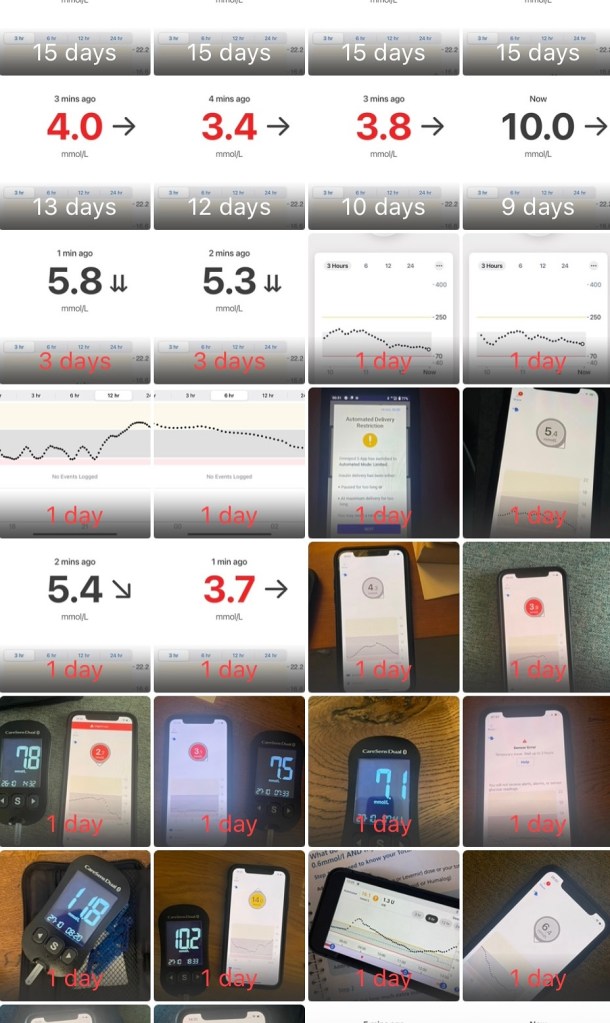
In the early days, we put so much pressure on ourselves to get it right all the time; thriving to hit the targets, avoid the hypo’s (low blood glucose levels) and hyper’s (high blood glucose levels). However, it wasn’t sustainable.
If I am being honest, I think that I felt the pressure more as a healthcare professional (currently on a career break). Quite a few people commented about how lucky T was to have a Dietitian as a mother. Full disclaimer, since qualifying as a dietitian I have done little in the world of diabetes other than supporting patients that may also have diabetes. If a patient with Type 1 Diabetes required input, they would always be signposted back to their specialist team. I specialise in oncology which is very different. Therefore, whilst people assumed that I knew a lot, all I needed was to be treated like a mother with no clue and limited knowledge.
What the numbers don’t show
The constant decisions – it is estimated that an extra 180 decisions a day are made for a Type 1 Diabetic (Stanford Medicine, 2014).
- Insulin timing
- Whether running about in play park is OK and not going to send levels plummeting
- Whether letting T have the birthday cake at the party is OK, never mind having to guess what the carb content of the cake is…. (still yet to get this one right)
The hypo’s avoided – the time in range may look good but it doesn’t show that having that having the target set to 6.1 mmol/L will sometimes cause the pump to over shoot, meaning that we need to step in and give dextrose tablets to prevent that hypo.
The interrupted sleep – waking up to the CGM alarm going off alerting you to a hypo and then having to wake your child up at 3am to give them dextrose tablets half asleep. I wake up most nights at least once a night to check what his levels are.
The constant maths – carb counting 5 times a day (T likes to eat). Eating out has become a source of stress, and trips to cafes and restaurants are no longer a thing. I’m not looking for sympathy as we are fortunate to be able to afford to eat out, but when you have to wait for the food to arrive to be able to guess the carb content before asking your child to look at it for 10 minutes whilst they wait to eat, it is just stressful and not really fair. The Italians also don’t do kids’ portions, and on one occasion, the bowl of pasta was never-ending and bigger than we originally thought. Cue meltdown in the restaurant as we were trying to get T to stop eating, as we hadn’t given enough insulin.
The finger pricks – because you don’t trust the CGM reading or it decided to stop working. Some days we do none and some days you run out of fingers to prick.
Changing insulin pumps and CGMs – this is done every 3 and 10 days respectively and whilst we know that it means he doesn’t have to have 6 injections a day, to a 5 year old it is rubbish.
The stress of waiting to eat – honestly, the frustration at having to wait 10 minutes is probably the biggest source of stress in our house. Before any snack or meal, T always questions how long he will have to wait to eat, even though he knows that it is 10 minutes. We have suggested things to fill the time (colouring/playing a game/watching an episode of a favourite programme) but it is always met with resistance.
Mental load and anxiety
- Decisions made (did I do the right thing?)
- Alarms going off in the middle of the night. It is a hypo or just a pressure low where he has been lying on his sensor?
- When diabetes just doesn’t want to play ball and you have been dealing with a stubborn hyper for 90 mins, give a bit more insulin, do some running around and then suddenly levels start to drop like a stone and you are then worried about a hypo
- The fact that you can do exactly the same thing two days in a row and get completely different results. I read somewhere that Type 1 Diabetes is like sitting an exam but by the time you have finished answering the questions, the questions have changed. Sounds about right…
The enforced activity – the 0830 trips to the play park on a Sunday morning as high glucose levels just won’t shift. Sometimes, a walk can be more effective at shifting those stubborn hyper’s

The guilt – when he is crying about how much he hates diabetes or if we have had to say ‘no, you can’t have that snack yet as your levels are too high’ or ‘no, you can’t run off and play yet as you are about to have a hypo’. As parents, I think it is safe to say that that we feel guilt and would do anything to take the hurt away from T.
I haven’t written this post to just complain or to make people feel sorry for us. I am writing it for the people also living the Type 1 Diabetes life to say that we see you and we get it.
For those not directly living it, it’s about raising awareness of Type 1 Diabetes, what it entails and to highlight that the number on the screen is only just the start.
Diabetes is a 24/7 job and a constant worry. We are 5 months into this lifelong journey and only starting to get to grips with things. Despite some days being harder than others, it never ceases to amaze us how resilient a 5 year old can be and at the end of the day, we still love a dance party (sorry to our neighbours for soda pop and zoo, the current favourite songs, for being on repeat).
L x



Leave a comment